Diabetic Foot
Introduction
Diabetic foot refers to a series of foot-related complications arising from uncontrolled diabetes. It is characterized by nerve damage (neuropathy) and poor blood flow (peripheral arterial disease) in the lower limbs, making the feet vulnerable to injuries and infections. If left untreated, diabetic foot can lead to severe complications, including foot ulcers, infections, and, in extreme cases, amputation.
I. Causes and Risk Factors Associated with Diabetic Foot
Diabetic foot is primarily caused by long-term, uncontrolled diabetes, particularly when blood sugar levels remain elevated for extended periods. High blood sugar levels can damage blood vessels and nerves, impairing the body’s ability to heal and fight infections. This combination of factors makes the feet susceptible to injuries and challenges in healing, leading to the development of diabetic foot complications.
Several factors contribute to the increased risk of developing diabetic foot among individuals with diabetes, including poor blood sugar control, foot deformities, inadequate foot care, chronic smoking, and uncontrolled hypertension.
II. Signs and Symptoms of Diabetic Foot
Diabetic foot often presents with several noticeable signs and symptoms that warrant attention. These include:
- Numbness or Tingling in the Feet: Diabetic neuropathy can cause sensations of numbness or tingling in the feet.
- Loss of Sensation in the Feet: As diabetic neuropathy progresses, it may lead to a complete loss of sensation in the feet.
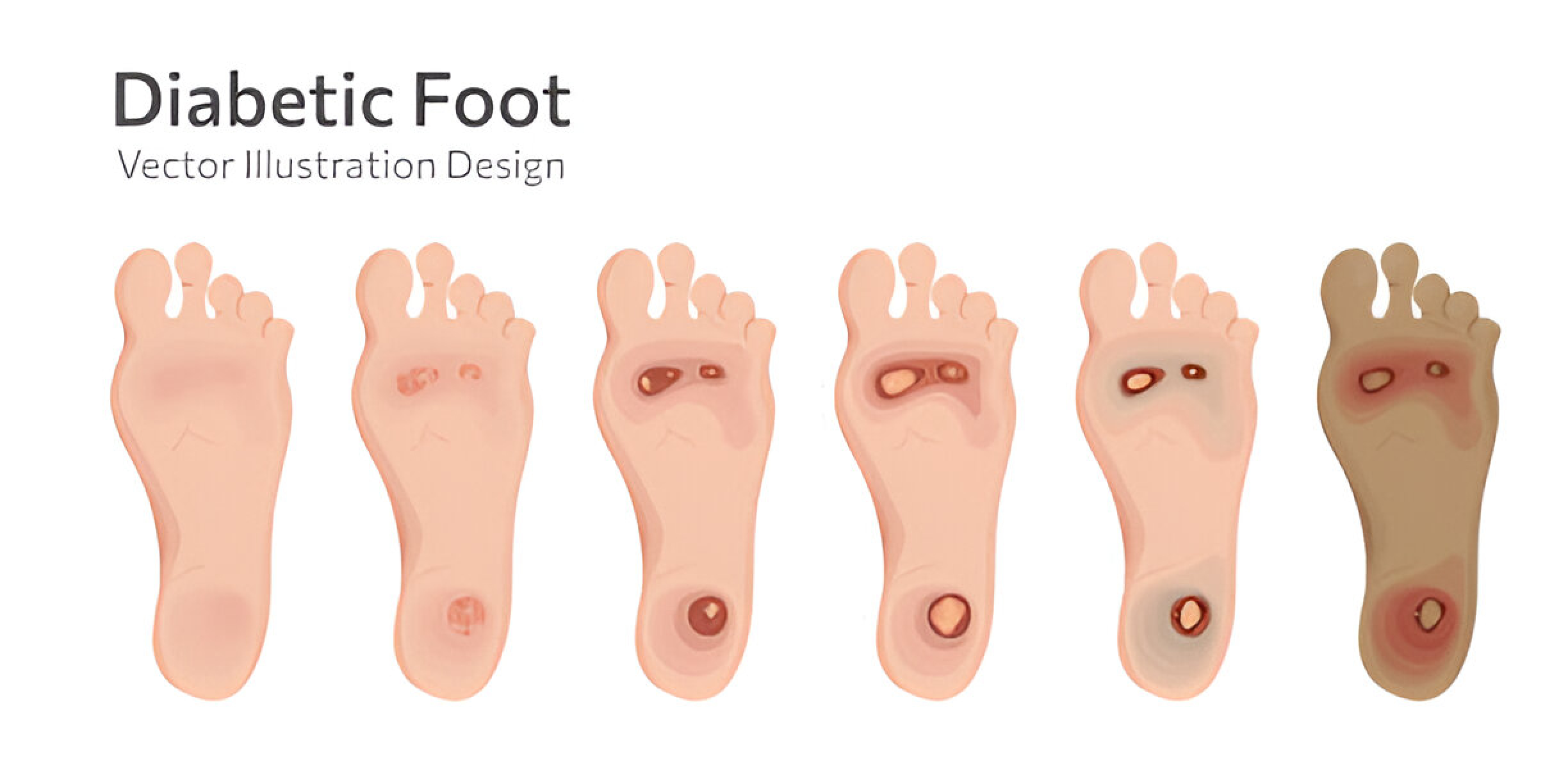
- Foot Ulcers: Diabetic foot ulcers are open sores or wounds that do not heal properly, often developing due to pressure points, trauma, or repetitive stress on the feet.
- Swollen Feet: Poor blood flow in the feet, a condition known as peripheral arterial disease (PAD), can cause swelling or edema in the lower extremities.
III. Diagnosis of Diabetic Foot
The diagnosis of diabetic foot involves a comprehensive assessment by healthcare professionals. This includes taking a detailed medical history and conducting a thorough physical examination of the feet. Additionally, specialized tests are employed to evaluate nerve and blood vessel function in the feet, aiding in accurate diagnosis and personalized treatment planning.
- Medical History and Physical Examination: The first step in diagnosing diabetic foot involves taking a detailed medical history, including the duration and control of diabetes, any previous foot issues, and lifestyle habits.
- Tests to Evaluate Nerve and Blood Vessel Function: Specialized tests such as nerve conduction studies and assessments of blood flow (ankle-brachial index and color Doppler) are used to evaluate nerve and blood vessel function.
By combining medical history, physical examination, and specialized tests, healthcare professionals can accurately diagnose diabetic foot and create individualized treatment plans. Early diagnosis allows for timely intervention, promoting better foot health and reducing the risk of severe complications. Regular foot check-ups and diligent foot care play a vital role in maintaining the well-being of individuals with diabetes.
IV. Treatment of Diabetic Foot
Effective management of diabetic foot requires a multi-faceted approach, which may include:
- Ulcer Debridement and Regular Dressing: This procedure involves the removal of all non-healing tissue, including necrotic and devitalized tissue and calluses around the wound, reducing plantar pressures and promoting the formation of granulation tissue and re-epithelialization.
- Optimization of Blood Sugar Levels: Keeping blood sugar levels within the desired range during diabetic foot treatment is crucial for allowing tissues to heal naturally, as higher blood glucose levels are associated with a lower inflammatory response and a weaker defense against infections.
- Medicine to Promote Better Blood Flow: To support healing, medical professionals may prescribe medicines that promote blood flow, as poor circulation can hinder natural healing and prevent ulcers from closing.
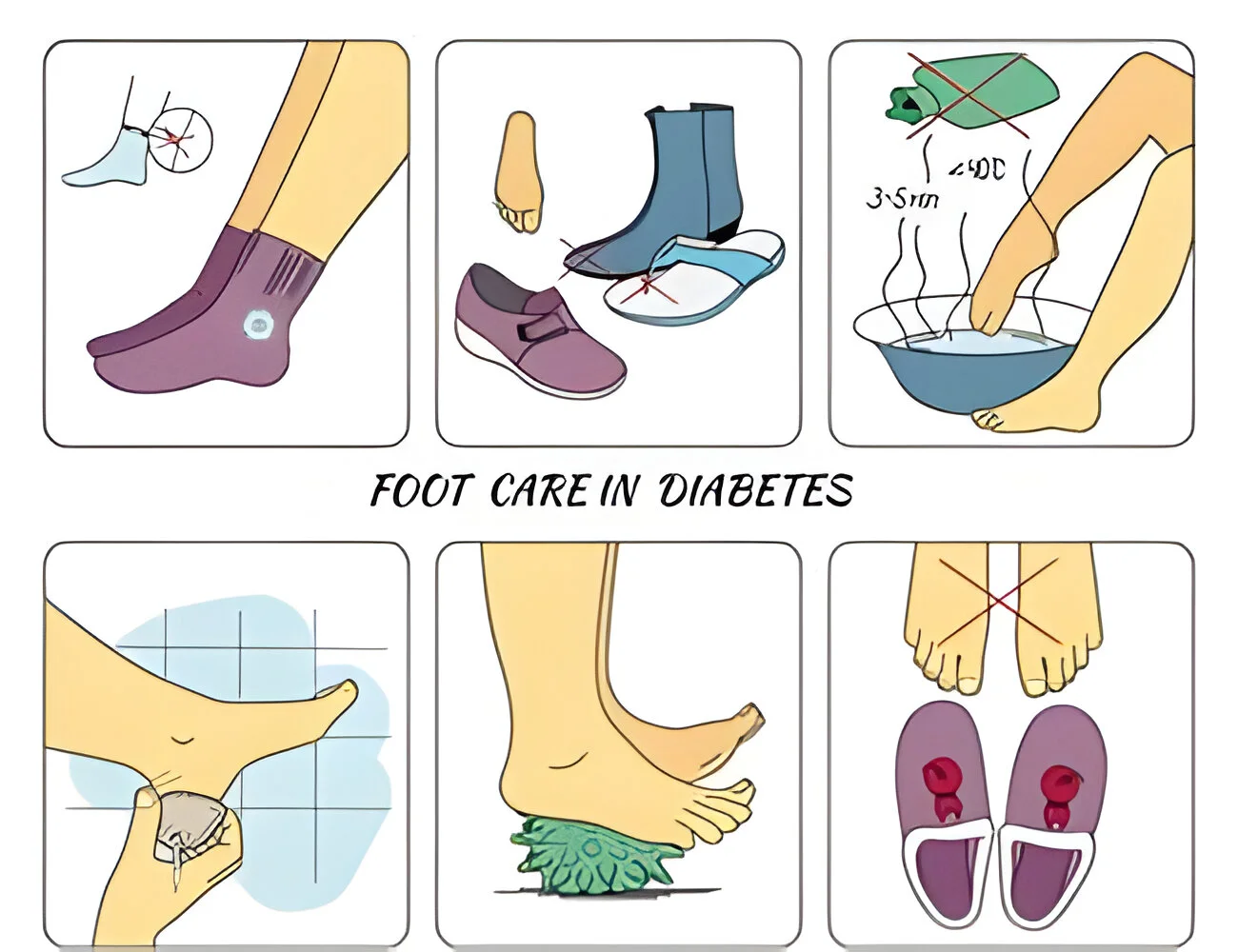
- Footwear for Pressure Point Offloading: Patients may be advised to wear offloading footwear designed to redistribute pressure in the feet, which can benefit those at risk for foot complications such as neuropathic ulcers, Charcot foot, and infection.
V. Prevention of Diabetic Foot
Preventing diabetic foot is essential to avoid potential complications. Key preventive measures include:
- Proper Foot Care: Regularly inspecting and caring for the feet can prevent minor problems from escalating.
- Regular Foot Examinations: Frequent foot check-ups by healthcare professionals can detect any issues early on.
- Monitoring and Controlling Blood Sugar Levels: Maintaining optimal blood sugar levels is crucial in preventing diabetic foot.
- Early Intervention: Addressing minor foot problems promptly can prevent their progression into more severe complications. Seek medical attention immediately for any foot issues.
- Healthy Lifestyle Habits: Adopting a balanced diet, regular exercise, and avoiding smoking can contribute to overall diabetes management.
VI. Complications of Diabetic Foot
Neglecting the management of diabetic foot can lead to severe complications, including:
- Infection: Diabetic foot ulcers are open wounds that do not heal properly and are susceptible to infections, as high blood sugar levels impair the body’s ability to fight off infections.
- Osteomyelitis: Diabetic foot infections can extend to the bones, causing osteomyelitis, a serious condition where the bones become infected and inflamed.
- Gangrene: Reduced blood flow to the feet due to peripheral arterial disease (PAD) can lead to tissue death (gangrene).
VII. Conclusion
Diabetic foot is a serious and potentially devastating complication of diabetes that demands proactive care and timely interventions. Early detection, proper management, and preventative measures are crucial in ensuring the well-being of individuals with diabetes. By focusing on foot care, regular check-ups, and maintaining healthy blood sugar levels, the risk of diabetic foot and its complications can be significantly reduced. Understanding the importance of preventing and treating diabetic foot is vital in safeguarding the quality of life and overall health of those affected by diabetes. Awareness and a proactive approach can lead to a healthier and happier future.

